AAC and Cerebral Palsy
The Role of High-Tech AAC in Supporting Communication for Individuals with Cerebral Palsy
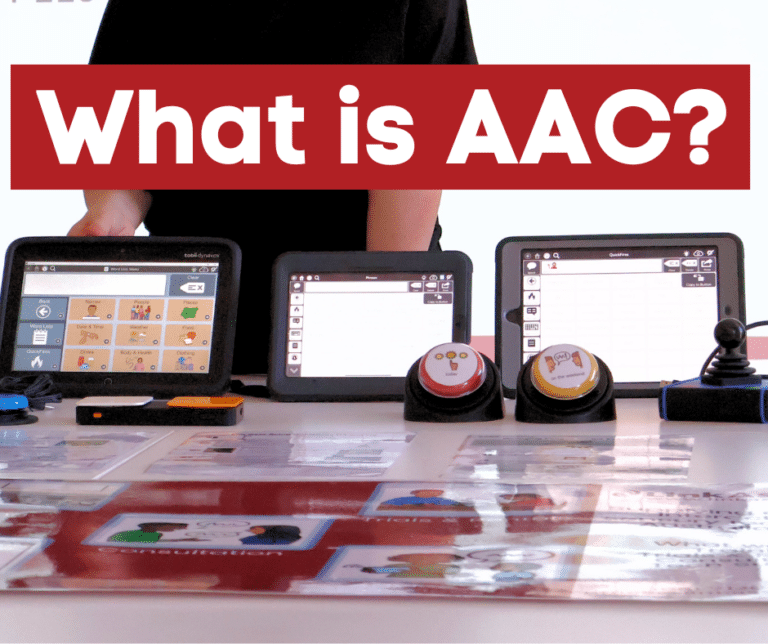
Cerebral palsy (CP) is a group of neurological disorders that affect movement, muscle tone, and posture. Many individuals with CP experience communication challenges due to motor impairments. High-tech Augmentative and Alternative Communication (AAC) systems offer vital support by enabling individuals with CP to communicate effectively, participate in daily life, and achieve greater independence.

*Infographic taken from World Cerebral Palsy Day website
How Can High-Tech AAC Help?
High-tech AAC refers to electronic communication aids, including speech-generating devices (SGDs), tablets, and smartphones equipped with specialized AAC software. These systems allow users to construct messages using text, symbols and/or photos, which are then spoken aloud by the device. The technology can be tailored to meet the unique physical and cognitive needs of each user.
For individuals with limited motor control, high-tech AAC systems can offer alternative access methods such as:
- Eye gaze technology: Enables users to control the device using eye movements.
- Switch access: Allows communication through single or multiple switches activated by any intentional movement.
- Adapted and alternative mice: Provide accessible input options for users with partial motor function (e.g. joystick control, trackball mice, head-controlled mice).
Customisation is essential to ensure the AAC system aligns with the user’s abilities and preferences. Vocabulary sets, interface layouts, and voice options can be adjusted to support meaningful and efficient communication.
Focus on Eye Gaze Technology
Eye gaze technology is a powerful form of high-tech AAC that can significantly enhance communication for individuals with CP, especially those with limited or no voluntary motor control of their limbs or speech muscles.
Eye gaze systems use infrared cameras and sensors to track where a person is looking on a screen. By focusing their gaze on specific symbols, letters, or words, users can select items and construct messages. These messages are then spoken aloud by the device, allowing for verbal communication without physical touch.
In 2021, clinical guidelines for eye gaze technology for people with CP were developed. These can be accessed here: Eye-gaze control technology for people with cerebral palsy. 2021 Clinical Guidelines – AusACPDM. The guidelines explore a range of clinical considerations for effective implementation of eye gaze technology for people with CP, including:
- Assessment of visual and cognitive abilities, including fixation, visual acuity, and perceptual skills.
- Proper seating and positioning, which are critical for accurate eye tracking.
- Support from a multidisciplinary team, including speech pathologists, occupational therapists, and caregivers.
- Training and practice, embedded in daily routines to build proficiency and reduce fatigue.
A trial period is essential to determine the suitability of eye gaze technology. During this phase:
- Utilise the supports provided by the device supplier, including clinical and technical support, during the trial period.
- Multiple devices and software programs should be tested for suitability.
- Goals should be set collaboratively with the user and their support network.
- Activities should be tailored to the user’s interests and abilities.
- Feedback should be gathered to refine device setup and usage strategies.
Resources
Professionals such as speech pathologists and occupational therapists play an essential role in guiding users through the selection, customisation, and ongoing adaptation of AAC and assistive technology. Useful assessment tools for professionals to have in their toolkit include:
- Identifying the technology needs of your client: Identifying Client Technology Needs Rating Scale
- Assessing your client’s current communication needs and goal setting: Dynamic AAC Goals Grid (DAGG-3) + instruction manual
- Access Screening Tool – a tool for helping you decide on an access method that may be suitable for someone: Access Screening Tool.pdf
- A list of access features to consider for your client: Access Features List
- Identifying the features required in an AAC device: TD AAC Feature Consideration Tool
- Feature Matching Tool: Considerations for Choosing a Communication Device
- Emergent Eye Gaze webinar: Emergent Eye Gaze: An Introduction – Link Assistive
Articles
Batorowicz, B., Stadskleiv, K., Renner, G., Dahlgren Sandberg, A., & von Tetzchner, S. (2018). Assessment of aided language comprehension and use in children and adolescents with severe speech and motor impairments. Augmentative and Alternative Communication, 34(1), 54–67. https://doi.org/10.1080/07434618.2017.1420689
Eyes on Communication Research Group. (2021). Eye-gaze control technology for people with cerebral palsy: Clinical guidelines (Version 1). Cerebral Palsy Alliance & The University of Sydney. https://doi.org/10.1186/s12883-021-02077-z
Hoopmann, L., Bailey, B., & Arciuli, J. (2024). Let the eyes do the talking: A scoping review of eye-tracking in paediatric communication assessment and intervention. International Journal of Speech-Language Pathology. Advance online publication. https://doi.org/10.1080/17549507.2024.2425012
Karlsson, P., Allsop, A., Dee-Price, B.-J., & Wallen, M. (2017). Eye-gaze control technology for children, adolescents and adults with cerebral palsy with significant physical disability: Findings from a systematic review. Developmental Neurorehabilitation. https://doi.org/10.1080/17518423.2017.1362057
Karlsson, P., Bech, A., Stone, H., Vale, C., Griffin, S., Monbaliu, E., & Wallen, M. (2019). Eyes on communication: Trialling eye-gaze control technology in young children with dyskinetic cerebral palsy. Developmental Neurorehabilitation, 22(2), 134–140. https://doi.org/10.1080/17518423.2018.1519609
Karlsson, P., Griffiths, T., Clarke, M. T., Monbaliu, E., Himmelmann, K., Bekteshi, S., Allsop, A., Pereksles, R., Galea, C., & Wallen, M. (2021). Stakeholder consensus for decision making in eye-gaze control technology for children, adolescents and adults with cerebral palsy service provision: Findings from a Delphi study. BMC Neurology, 21(63). https://doi.org/10.1186/s12883-021-02077-z
Perfect, E., Hoskin, E., Noyek, S., & Davies, T. C. (2020). A systematic review investigating outcome measures and uptake barriers when children and youth with complex disabilities use eye gaze assistive technology. Developmental Neurorehabilitation, 23(3), 145–159. https://doi.org/10.1080/17518423.2019.1600066
Smith, A. L., & Hustad, K. C. (2015). AAC and early intervention for children with cerebral palsy: Parent perceptions and child risk factors. Augmentative and Alternative Communication, 31(4), 336–350. https://doi.org/10.3109/07434618.2015.1084373
Stevens-Hofer, B., Wallen, M., McInerney, M., & Karlsson, P. (2024). Eyes on communication: Strategies to facilitate uptake of clinical practice guidelines for implementation of eye-gaze control technology by people with cerebral palsy. Disability and Rehabilitation: Assistive Technology. Advance online publication. https://doi.org/10.1080/17483107.2024.2437142
Vivanti, G. (2019). Eye-gaze control technology holds the potential to promote communication skills in young children with dyskinetic cerebral palsy, but more rigorous research is needed to prove its effectiveness. Evidence-Based Communication Assessment and Intervention, 13(4), 210–212. https://doi.org/10.1080/17489539.2019.1653006
Wallen, M., & Karlsson, P. (2023, March 7). Eyes on Communication: Strategies to facilitate uptake of clinical practice guidelines for implementation of eye-gaze control technology by people with cerebral palsy [Summary report]. Cerebral Palsy Alliance.